Over time, diabetes may affect many areas of the body. The eyes are no exception. Diabetes can produce varying degrees of vision loss. Diabetes threatens vision because it may damage the retina, the delicate inner lining that sends visual messages to the brain. Diabetic retinopathy, is “silent” with no outward symptoms in its early stages. It’s not until the later stages that vision loss is noticeable.
Anyone who has had diabetes for more than 10 years is a prime target for diabetic retinopathy. Detected early, it can be monitored and treated most of the time. Left untreated, it may lead to blindness.
THE EYES ARE THE WINDOW TO THE BODY
The retina is a fragile and transparent membrane. It contains tiny blood vessels that provide it with nutrition. Diabetic retinopathy weakens these vessels, causing blood to leak into the surrounding tissue.
When this happens, the retina swells up; and vision is affected. If these changes are occurring in the eye, there is a high probability that they are also occurring in other body organs, such as the kidneys or feet. That’s why the eyes are often referred to as “the window to the body.”
This swelling is only one complication of retinopathy. The retina can also develop abnormal vessels and scar tissue, causing it to function improperly. The abnormal blood vessels are fragile. If the vessels burst, blood will fill the back of the eye and prevent light from reaching the retina. The result is loss of vision.
Below are diagrams of a normal eye and a diabetic eye. Notice the differences. 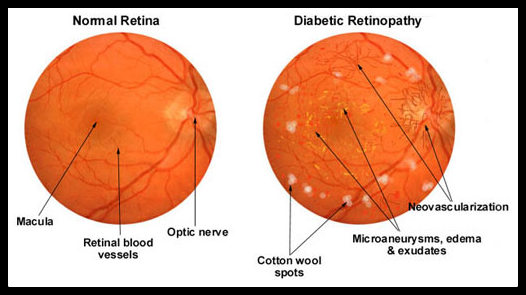
TREATMENT OF DIABETIC RETINOPATHY
In many cases, diabetic retinopathy can be treated before vision loss occurs. Laser treatment is highly successful in halting the progress of the disease. A beam of laser light is directed into the eye to seal the source of leakage and repair the damaged area. While it can improve vision, it cannot reverse scarring of the retina.
Not all stages of retinopathy require laser surgery. At every stage, however, testing should occur to make sure fluids are not leaking into the retina. Diabetics are encouraged to have a dilated retinal exam and/or digital retinal photography at least once a year.
This is an eye after laser treatment for diabetic retinopathy (bleeding). The laser literally burns the retina at the origin of the bleed, causing scar tissue which in turn stops (seals) the bleeding.
VISION CHANGES
Many times, one of the first signs of diabetes is vision fluctuation. You’ll get a new pair of glasses, and they only seem to work for a short while, or they don’t work at all. If you find that your vision changes suddenly and you are feeling excessively tired or very thirsty or urinating frequently, this could be an early indicator that your blood sugar is off.
PREVENTION OF DIABETIC RETINOPATHY
Early detection and treatment are the keys to preventing loss of vision. Stability of your sugar levels is most critical in preventing diabetic changes. We recommend small frequent meals at roughly the same time each day. We have seen patients who have had diabetes for 25 years with no eye complications. Conversely, we have seen patients who have had diabetes for 5 years who have significant diabetic eye disease. Most diabetics will develop some form of diabetic retinopathy. That’s why constant evaluation is so critical.
In the early stages, diabetic retinopathy is unnoticeable. You won’t experience pain or blurring or even be aware you have a problem. It’s important for your eyes to be examined so that any diabetic changes that need attention can be properly documented (photographed) and/or treated before they cause symptoms.
If you are diabetic, an exam is recommended each year. If you have poor control of your blood glucose levels, high blood pressure, or protein in the urine, exams should be more frequent.